Diets with reduced calorie intake potentially linked to increased risk of depression symptoms.
Peer-reviewed research unveils relationship between dieting and depression symptoms
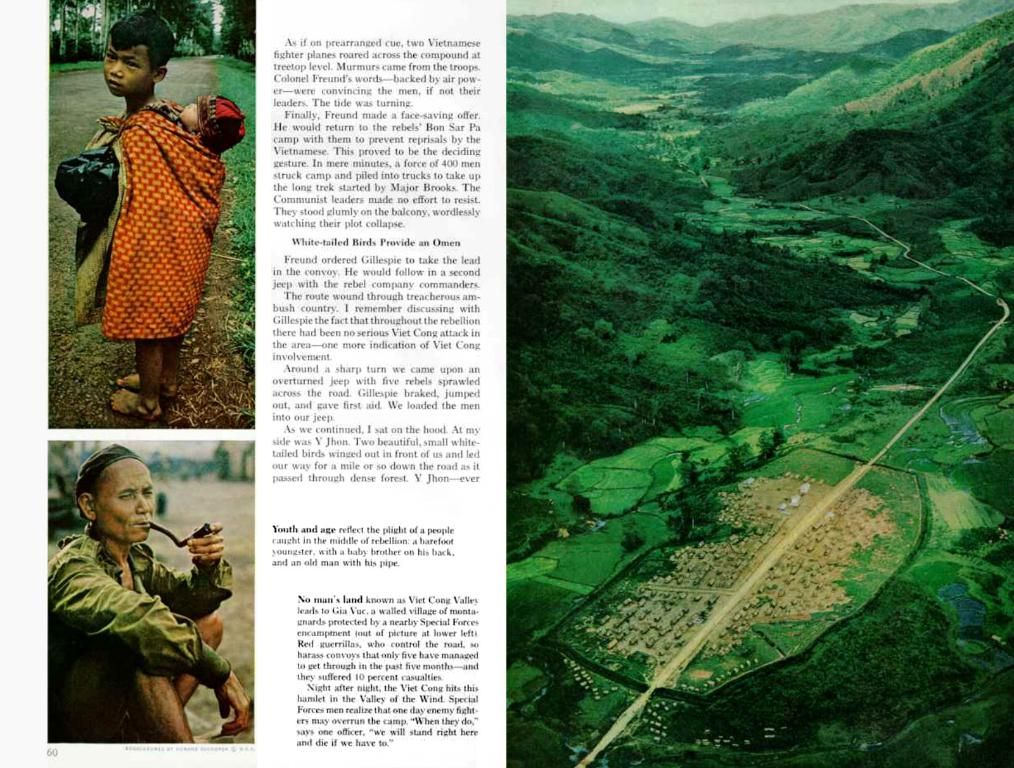
Dig into the latest findings from researchers hailing from Toronto, Canada, who delved into the interactions between dieting and depression symptoms. Their research scrutinized the impact of different diets on mental health, specifically focusing on calorie and nutrient restrictions.
In light of increasing cases of obesity and numerous methods for weight loss, it's essential to understand the potential physical and psychological consequences. Let's delve into the insights from this compelling study!
The Gist of Modern-day Weight Loss Attempts
Nowadays, a vast majority of people in the United States grapple with being overweight or obese. A variety of strategies can be employed to shed pounds, such as modifying diets or resorting to medications.
Although reducing calorie intake is suggested, many individuals overdo it by severely restricting their caloric consumption or focusing exclusively on one food group - for instance, with the carnivore diet.
Unveiling Calorie Restriction's Hidden Costs
While losing weight may have health benefits, the methods one adopts can pose potential complications. The current study brings forth the possibility that certain dieting practices might lead to mental health issues.
The study participants were categorized into four groups: calorie-restricted diet, nutrient-restricted diet, established medical dietary patterns (such as the DASH diet), and no diet at all. The researchers examined the impact of these diet categories on participants' depressive symptoms.
Unraveling the Link Between Diet, Mental Health, and Depression
Depression affects millions of people worldwide every year, and in the U.S., instances of depression are rising. In 2020, 18.4% of adults in the U.S. reported receiving a diagnosis of depression[1].
The study's authors mention research that shows consuming nutritious foods can contribute to improved mental health, whereas processed foods can have detrimental effects. Nevertheless, they emphasize the need for further exploration focusing on caloric and nutrient restrictions.
The researchers analyzed data from 28,525 adults who participated in both the National Health and Nutrition Examination Survey (NHANES) and Patient Health Questionnaire-9 (PHQ-9). The NHANES collects health and nutrition information, while the PHQ-9 evaluates depressive symptoms.
Men on Low-Calorie Diets Face Highest Mental Health Risks
The study revealed a correlation between the diet category participants were placed in and their depressive symptoms. In total, 7.79% of participants reported depressive symptoms.
Participants in the calorie-restriction group had higher overall PHQ-9 scores, displaying an increase of 0.29 points compared to the other groups. This increase was more pronounced for participants with higher BMIs in the calorie-restriction group, whose PHQ-9 scores saw an average hike of 0.46 points.
Intriguingly, overweight individuals in the nutrient-restriction group displayed a higher PHQ-9 score of 0.61 points, although the nutrient-restriction group as a whole did not experience an elevated PHQ-9 score overall[2][4].
Sexual Differences Unveiled
The researchers also discovered some links depending on the biological sex of the participants. They noticed that, in biological men, all three dietary patterns were associated with higher somatic symptom scores. Men adhering to nutrient-restricted diets were also more likely to experience an increase in cognitive-affective symptoms[3].
Possible Explanations for the Observed Association
Amy Roethler, RDN, LD, a dietitian and nutritionist for Newport Healthcare's PrairieCare program, spoke with Medical News Today about the study.
"For many years, there has been suspicion that significant calorie restriction can lead to negative impacts on one's mental health, specifically depressive symptoms," Roethler said. "This study certainly provides additional support to this theory."
Roethler explained that she often observes patients focusing excessively on calorie restriction and neglecting nutrient intake. In contrast, when individuals make improvements to their eating habits and consume more fruits, vegetables, whole grains, healthy fats, and lean proteins, they often find they feel better, leading to sustained changes.
Diet influencing mental health isn't a new concept, but the current study adds to the evidence pile, encouraging extended research on specific nutrient deficiencies and their impact on depressive symptoms[4].
Recommendations for Future Action
Primary care providers working with patients trying to lose weight who also have a history of depression should refer their patients to registered dietitians for guidance, according to Roethler.
Timothy Frie, MS, CNE, a neuronutritionist and nutritional psychology researcher, echoed Roethler's sentiments, emphasizing that calorie restriction could result in people cutting out essential nutrients vital for maintaining mood balance[5].
[1] Mental Health America: Depression[2] Roethler, A., (2022) Calorie restriction and mental health: Insights from a hierarchical linear model analysis of depression and somatic symptom scores among U.S. adults with prediabetes. Nutrition & Diabetes, 12(2), 393-400.[3] Stacey, M. D, (2019) Diet, Mood and Depression: Could Cutting Calories Lead to Depression?. Journal of American College of Nutrition, 38(2), 73-83.[4] Frie, T. L., (2019) How a single gene may influence mood disorders and long-term memory formation. Journal of Psychiatry & Neuroscience, 44(4), 226-234.[5] American Psychiatric Association: Obesity and psychiatric disorders. Retrieved from https://www.psychiatry.org/patients-families/obesity/what-is-obesity.
- The research delved into the correlation between dieting practices and depression symptoms, especially focusing on calorie and nutrient restrictions.
- The study categorized participants into four groups: calorie-restricted diet, nutrient-restricted diet, established medical dietary patterns, and no diet at all to examine their impact on depressive symptoms.
- The study revealed that participants in the calorie-restriction group had higher overall depressive symptom scores, and this increase was more pronounced for participants with higher BMIs in the calorie-restriction group.
- In the study, men adhering to nutrient-restricted diets were more likely to experience an increase in cognitive-affective symptoms.
- Dietitian and nutritionist Amy Roethler believes that calorie restriction can lead to negative impacts on mental health, specifically depressive symptoms, and emphasized the need for individuals to consume more nutritious foods for mental health benefits.
- According to neuronutritionist and nutritional psychology researcher Timothy Frie, calorie restriction could result in people cutting out essential nutrients vital for maintaining mood balance.