Thumb Hyperflexibility: Understanding Signs, Root Causes, and Beyond
Joint Hypermobility: Understanding a Common yet Complex Condition
Joint hypermobility is a relatively common condition that affects approximately 10 to 25% of the general population [1]. Most individuals with hypermobile joints do not experience significant problems, but a minority suffer from symptoms and complications related to the condition.
What is Joint Hypermobility?
Joint hypermobility refers to the ability of joints to move beyond their normal range of motion. According to the Brighton criteria, a person has joint hypermobility if they have two major criteria, one major and two minor criteria, four minor criteria, two minor criteria and a close relative, such as a parent, has joint hypermobility [2].
Associated Conditions and Complications
When joint hypermobility causes pain and other symptoms but does not meet criteria for genetic connective tissue disorders, it is termed Hypermobility Spectrum Disorder (HSD) [1][2]. Symptoms can include frequent joint dislocations, chronic pain, and early onset osteoarthritis [2].
Ehlers-Danlos Syndrome, Hypermobile Type (hEDS) is a heritable connective tissue disorder characterized by generalized joint hypermobility, frequent joint subluxations/dislocations, chronic musculoskeletal pain, and skin features like softness and easy bruising. It affects about 1 in 5,000 people globally and is the most common EDS subtype [1][5].
People with hypermobility may develop musculoskeletal complications such as flat feet, scoliosis, kyphosis, balance problems, early osteoarthritis, and frequent joint injuries due to instability [2]. They may also experience circulatory and digestive problems, have a tendency to poor wound healing, increased bleeding during childbirth, and higher risk of postpartum depression [2][5].
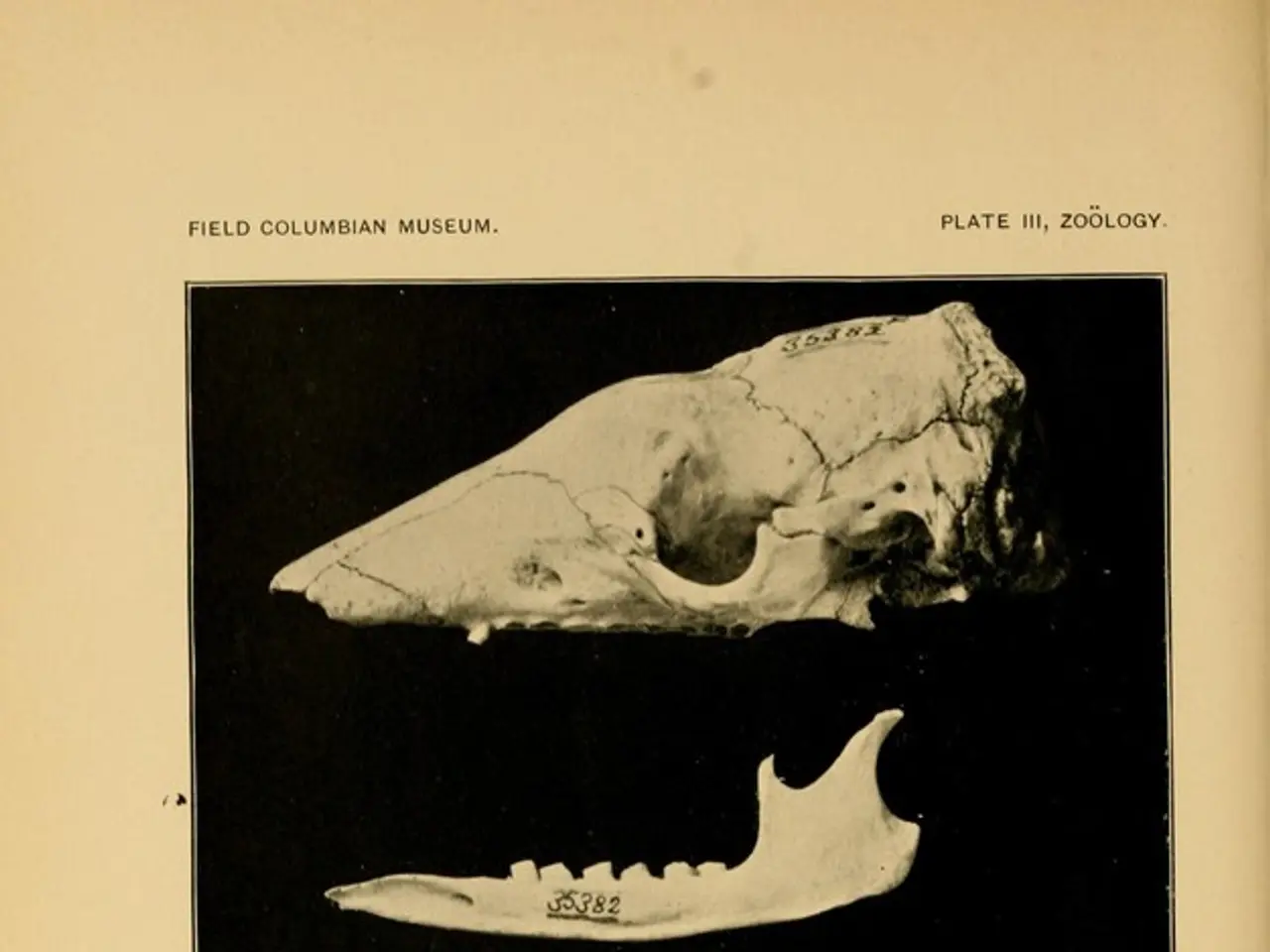
Temporomandibular Joint Disorders (TMD) are more prevalent among people with hEDS and HSD, possibly due to joint instability affecting the jaw [3].
Diagnosis and Management
While hEDS is genetic, it currently lacks a confirmatory DNA test, and diagnosis is clinical, based on joint assessment (e.g., Beighton score), symptoms, and family history. HSD is diagnosed when hypermobility symptoms are present but without a known heritable connective tissue disorder [1][2][5].
Management strategies for chronic pain associated with joint hypermobility include physical therapy, pain-relieving medications, and durable medical equipment such as cushions, compressive garments, and braces. Treatment for those with more severe symptoms mainly focuses on improving muscle strength to protect the thumb joints, which can help in decreasing pain, reducing the risk of dislocations, and improving muscle strength and fitness [6].
Conclusion
Joint hypermobility is a common condition that can lead to complications, particularly when it is part of a syndrome such as hEDS or HSD. Regular monitoring and management are important for affected individuals to help manage symptoms and improve quality of life.
References:
[1] Hypermobility Spectrum Disorders. (2021). Genetics Home Reference. https://ghr.nlm.nih.gov/condition/hypermobility-spectrum-disorders
[2] Hypermobility Syndrome. (2021). NHS. https://www.nhs.uk/conditions/hypermobility-syndrome/
[3] Temporomandibular Disorders. (2021). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/temporomandibular-disorders/symptoms-causes/syc-20355887
[4] Ehlers-Danlos Syndrome. (2021). Genetics Home Reference. https://ghr.nlm.nih.gov/condition/ehlers-danlos-syndrome
[5] Ehlers-Danlos Syndrome, Hypermobile Type. (2021). Genetics Home Reference. https://ghr.nlm.nih.gov/condition/ehlers-danlos-syndrome-hypermobile-type
[6] Management of Chronic Pain Associated with Joint Hypermobility. (2021). Arthritis Foundation. https://www.arthritis.org/living-with-arthritis/treatments/pain-management/pain-relief-options/joint-pain/joint-pain-treatment-options/management-of-chronic-pain-associated-with-joint-hypermobility.php
- Science has shed light on the complexities of joint hypermobility, a common condition affecting 10-25% of the population.
- Impotence in understanding this condition can lead to the undervaluing of its associated medical conditions and complications.
- Erectile dysfunction is not directly related to joint hypermobility, but it is essential to consider it when discussing mental health, as stress and anxiety can exacerbate symptoms.
- Chronic diseases, such as cancer, respiratory conditions, and digestive health issues, can coexist with joint hypermobility, necessitating multidisciplinary approaches to treatment and management.
- Eye health, hearing, and skin conditions may not be the primary focus in individuals with joint hypermobility, but they should not be overlooked, considering their impact on overall health and wellness.
- Fitness and exercise play a crucial role in managing joint hypermobility, as they can strengthen muscles and improve joint stability, reducing symptoms and preventing complications.
- Autoimmune disorders can accompany joint hypermobility, requiring specialized therapies and treatments for proper management.
- Nutrition plays a vital role in supporting cardiovascular health, which can be affected by joint hypermobility and its underlying conditions, such as chronic pain and osteoarthritis.
- CBD has demonstrated potential benefits for managing pain and inflammation associated with joint hypermobility, although more research is needed to determine its efficacy and safety.
- Neurological disorders may be more prevalent in people with joint hypermobility, making a comprehensive evaluation of their health essential.
- Skin-care practices should be tailored to address the specific skin conditions common in those with joint hypermobility, such as easy bruising and fragile skin.