What is asked for the Hungarian translation of "Appendicitis"?
In the midst of the COVID-19 pandemic, a pressing issue has come to light: the lack of language equity in healthcare for millions of individuals with limited English proficiency (LEP). This article explores the consequences of this disparity, the role of medical interpreters, and the need for system-wide change.
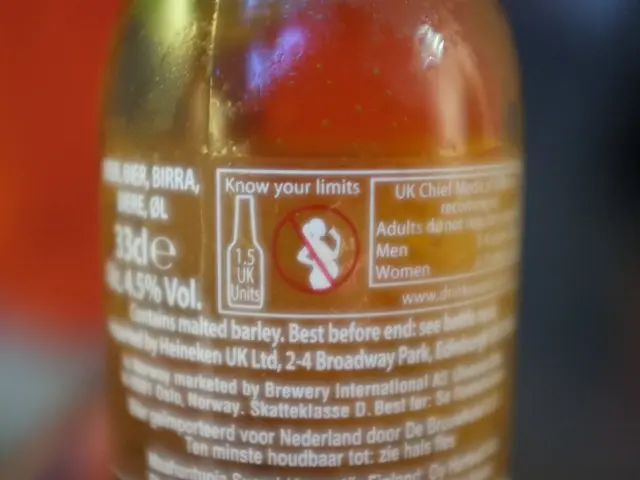
Vincent LaBarca, a DNP, NP-C, has firsthand experience with the challenges faced by LEP patients. In 2017, while in Budapest, Hungary, LaBarca, the author of this piece, experienced symptoms that led to a stay at a military hospital due to a ruptured appendix. Despite being in a foreign country, LaBarca felt unheard and isolated due to language barriers.
This sense of isolation and disconnection is a common experience for LEP patients. Poor outcomes in LEP patients are well-documented, including deferring care more often, higher risks of leaving the hospital against medical advice, fewer preventative services, and longer length of stays, particularly in the context of inpatient appendicitis treatment.
The pandemic has disproportionately affected non-English speaking patients, particularly those from Latinx communities. Surprisingly, the lack of coverage of language inequity during this critical period has been noticeable.
The threat to one's sense of self is acute in the presence of illness, and patients with LEP rightly feel disrespected, afraid, and frustrated when they are met with the medical gaze without proper communication.
Hospital administrators, insurers, lawmakers, and outside groups must work together to achieve system-level change for LEP patients. In some hospitals, nearly half of patients with LEP do not interact with an interpreter, highlighting the need for improved language access.
California, with its 1.7 million people with LEP, had less than 800 certified medical interpreters in 2015. These professionals are often underpaid and overworked, feeling "disposable" in the eyes of their clinical colleagues.
Organisations such as the Linguistic Access Network and the National Council on Interpreting in Health Care (NCIHC) are working to improve language access for LEP patients in the USA. Clinicians must not limit themselves to institutional responses to this phenomenological problem and must preserve their patients' sense of identity by taking steps such as expanding interpreter services and committing to those marginalized by political and economic forces.
With approximately 25 million people in the US with LEP, it is crucial to address this issue to ensure equitable healthcare for all. This article serves as a call to action for the healthcare community to prioritise language equity and work towards a more inclusive and just healthcare system.
Read also:
- Honoring Ayurveda Day 2024: Tapping into the Power of AYUSH for Worldwide Wellbeing
- casesof West Nile virus resulting in fatalities in Greece, with seven individuals confirmed to have succumbed to the disease
- Nutrient-Packed Wonders: Why Sardines Deserve Respect for Their Health Benefits
- Assessing the Importance: Deciphering the Meaning Behind an Attention Deficit Hyperactivity Disorder (ADHD) Diagnostic Examination